Breaking Stigma: Words That Hurt vs. Heal
A guide to mental health literacy and dignity-centered language.
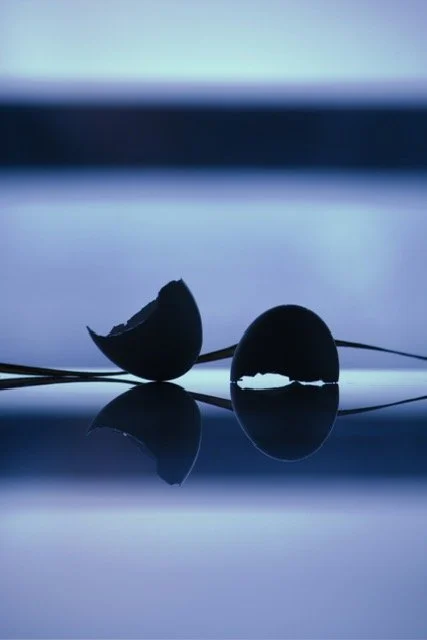
Sometimes what breaks us open is what lets the light in.
Have you ever casually called a messy situation "crazy" or described an organized friend as "so OCD"? We all use language thoughtlessly sometimes.
But when it comes to mental health, words carry real weight. They can either support healing or inflict measurable psychological damage. Language is a primary driver of stigma, actively discouraging people from seeking help and perpetuating fear.
This isn't about political correctness; it's about public awareness and respect. Thus, drawing on evidence-based research, this post explores three categories of language that are hurtful, and shows how choosing validating language that emphasizes dignity can pave the way toward a more compassionate society and support trauma-informed care. [1]
The most pervasive harm often comes from words we don’t even notice we’re using. Let’s explore further.
1. The Insidious Nature
A 2024 study on mental health literacy suggests that harmful language actively contributes to public stigma by trivializing serious conditions and equating mental illness with humor, weakness, or failure. Overtly Harmful Slang including terms like "crazy," "insane," "psycho," and "lunatic" reinforce sensationalized, negative stereotypes.
There is also the trivializing Insult that occurs when we use clinical diagnoses as casual adjectives. Calling a tidy person "OCD" or saying you're "depressed" over a minor disappointment trivializes the debilitating reality of these conditions for those who live with them.
2. Fear and Blame
When we use language that emphasizes danger or incompetence, we intensify fear. Stigma around serious mental illnesses (SMI), like schizophrenia and substance use disorders (SUDs), is strongly linked to the perception of a person being dangerous or personally at fault.
Linking Illness to Violence: Phrases that imply a person with a mental illness is inherently violent are deeply stigmatizing. Alarmingly, US trends tracked from 1996 to 2018 show an increase in public perception of likely violence toward people with schizophrenia, underscoring the urgency of changing this narrative.[1]
Focusing on Blame: When we frame symptoms, particularly those related to addiction, as a failure of willpower or a "bad character," it increases public anger and decreases empathy. This harmful rhetoric shifts the focus from a medical challenge to a moral failing.
Now that we understand what harms, let's explore how to do better.
3. Labels vs Validation
When we use language that emphasizes danger or incompetence, we intensify fear. Stigma is strongly linked to the perception of a person being dangerous or personally at fault.
The core concept in reducing mental health stigma is a simple, yet profound, use of dignity-centered language.
This strategy moves the focus from defining a person by their diagnosis to acknowledging that the illness is something they have, not something they are. To promote dignity, we must focus on the individual first, rather than the condition.
AVOID: Stigmatizing Language
Avoid using language that defines or limits an individual based solely on their diagnosis:
Group Labels: Avoid sweeping, generalizing labels like “The Mentally Ill.”
Diagnosis as Noun: Instead of “He is a schizophrenic” or “She is an addict.”
Passive Suffering: Avoid language that implies passive suffering or a constant battle, such as saying someone “Suffers from depression” or is “Battling his illness.”
Note: Some individuals describe their own experience as “battling” or “suffering,” and that’s their valid self-description. The concern is when others impose this language, stripping away agency and resilience.
USE: Dignity-Centered Language
Use language that maintains the dignity and wholeness of the individual:
Group Descriptions: Use compassionate, descriptive phrases, such as “People with a mental illness/condition.”
Focus on the Person: Say “He has schizophrenia” or “She has a substance use disorder.”
Active Resilience: Use empowering language that recognizes management and resilience, such as “Lives with depression” or “Is managing his condition.”
4. Stigma in Healthcare
Many providers suffer in silence, fearing that disclosing a mental health condition will lead to being viewed as “occupationally impaired,” a key driver of hidden self-stigma in healthcare.
Stigmatizing language isn’t limited to the general public; it pervades the healthcare system itself, with serious consequences for both providers and patients.
Provider Self-Stigma
Many providers worry that disclosing a mental health condition will lead to being viewed as “occupationally impaired,” risking their careers and reputation. These fears such as being barred from certain specialties or losing hospital privileges, forces many to associate psychological distress with weakness or shame, preventing them from seeking the very care they provide to others.
Clinical Insight
One of the most insidious forms of provider stigma is the dismissal of a patient’s valid experience. The body’s fight, flight, or freeze system doesn’t differentiate between a physical threat and a social or emotional one, and social rejection activates the same threat response.
When a provider minimizes a patient’s reaction to a threat, it can be perceived as an attack. Invalidation is re-traumatizing, underscoring why language is never “just words.”
Studies show that stigmatizing attitudes and the use of invalidated words are still common among healthcare workers, actively eroding patient trust.[2][3]
Stigma is a profound barrier to treatment, recovery, and a life of dignity. Reducing it starts with conscious reflection on the words we use every day.
By choosing dignity-centered speech, avoiding the casual use of clinical terms as insults, and challenging language that links mental illness to violence, we can all play a role in creating a more compassionate, informed, and healing environment.
I work with people who feel unseen and dismissed and help restore their self of agency. The antidote to that feeling is validation and connection to your inner strength.
if you are ready to have a judgment-free conservation, check out my Service page for more information. To start the inner work now, explore our free journal prompts listed below.
Journal Prompts:
The antidote to stigma is validation and connection. Start the path toward healing by taking time for quiet reflection and affirming your own reality.
What feeling comes up in your body when you hear a condition you live with being used as a casual insult (e.g., “psycho” or “OCD”)?
Where in your life have you encountered provider-based stigma (feeling dismissed or minimized) and how did your body react?
What is one stigmatizing term you’re going to commit to replacing with Person-First language this week?
Reclaiming Connection
If reading about stigma felt triggering, it’s because invalidation wounds your core human needs. The feeling of being unseen, dismissed, or judged is a deep survival threat.
The path to healing begins by affirming your own reality. We dive into this essential next step in our full Dear Needs series, where we explore how to rebuild the sense of belonging and validation that stigma erodes.
→ Continue Reading: [Dear Connection] (A reflection on connection, belonging, and reclaiming the validation you deserve.)
References
For a list of all cited research, view Citations here.
Ready to talk? / ¿Lista(o) para hablar?
English:
• Trauma-informed, integrated psychiatric care
• Non-controlled medication management
• For adults, teens, and children ages 6+
Español:
• Atención psiquiátrica integrada y con enfoque en trauma
• Manejo de medicamentos no controlados
• Para adultos, adolescentes y niños a partir de los 6 años
*This blog is for educational purposes only and does not constitute medical advice or establish a provider–client relationship.*
*Este blog es solo para fines educativos y no constituye asesoramiento médico ni establece una relación proveedor–paciente.*